Effets secondaires liés aux maladies et aux vaccins
 Un enfant peut aujourd’hui être vacciné contre plus de 11 maladies avant ses deux ans en France, au Belgique ou au Québec.. Cela peut bien sûr varier dans le monde, car tous les pays ne sont pas confrontés ni aux mêmes maladies ni aux mêmes enjeux sociaux. Pour chacune de ces maladies, les taux d’infection et de mortalité ont diminué de quasiment 100 % suite à la mise en circulation des vaccins1. De plus, étant donné que la plupart des personnes sont vaccinées, les épidémies aujourd’hui restent rares et rapidement contenues.
Un enfant peut aujourd’hui être vacciné contre plus de 11 maladies avant ses deux ans en France, au Belgique ou au Québec.. Cela peut bien sûr varier dans le monde, car tous les pays ne sont pas confrontés ni aux mêmes maladies ni aux mêmes enjeux sociaux. Pour chacune de ces maladies, les taux d’infection et de mortalité ont diminué de quasiment 100 % suite à la mise en circulation des vaccins1. De plus, étant donné que la plupart des personnes sont vaccinées, les épidémies aujourd’hui restent rares et rapidement contenues.
Ne vaut-il pas mieux obtenir l’immunité naturellement, c’est à dire en attrapant la maladie plutôt que via un vaccin?
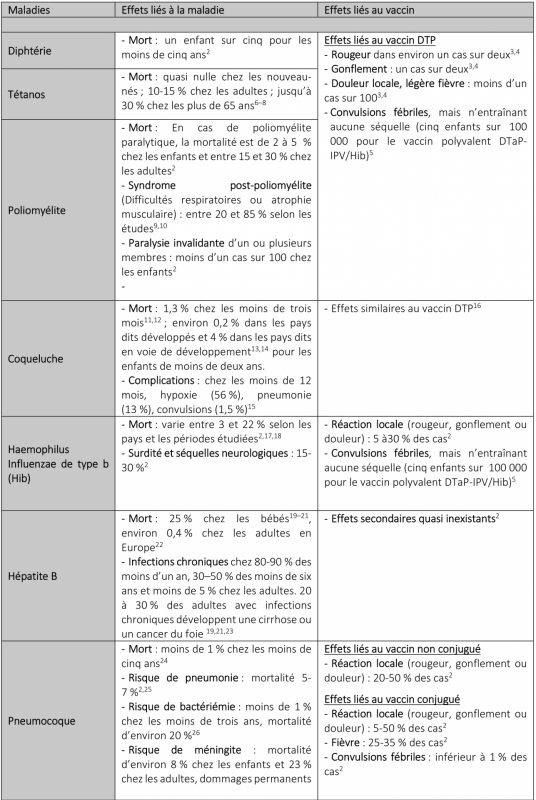
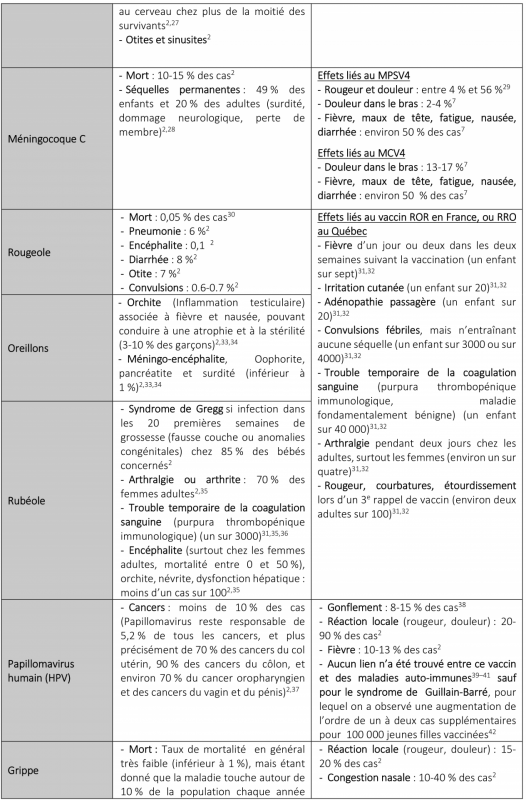
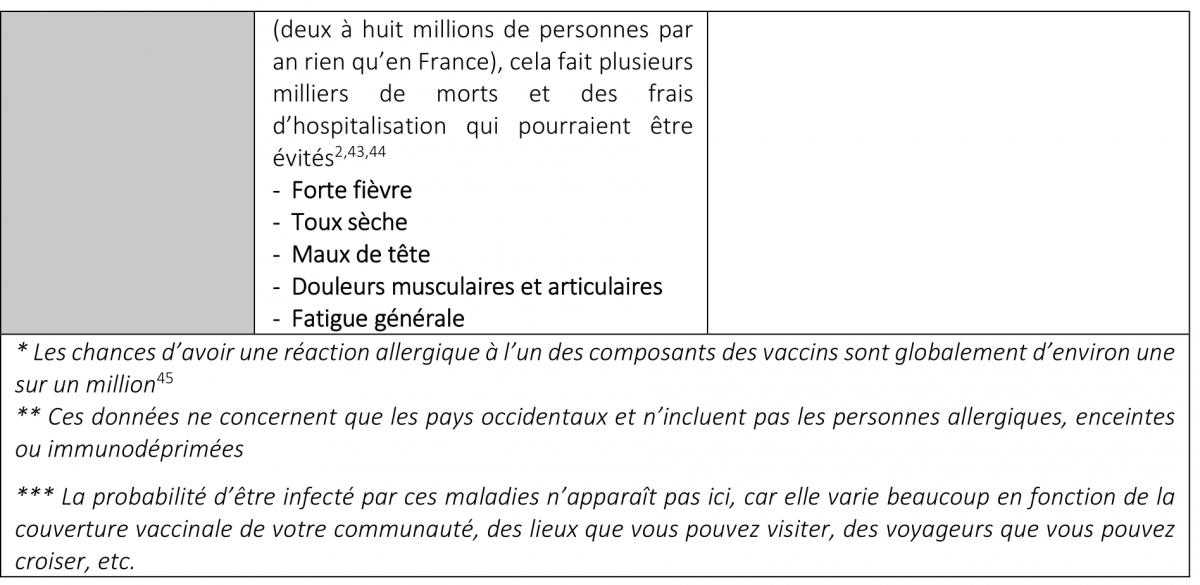
Lors d’une infection, notre système immunitaire répond en développant des cellules immunitaires produisant des anticorps adaptés à l’agent pathogène en cause. Ces cellules resteront ensuite dans le corps, prêtes à répondre rapidement à une infection similaire au cours de la vie. Mais, il faut noter que cette immunité « naturelle » peut coûter cher à l’individu à cause des complications que peut entraîner la maladie (voir tableau ci-dessous). Les vaccins, quant à eux, induisent aussi une immunité, mais de manière beaucoup plus douce. Le vaccin contient des composants infectieux de la bactérie ou du virus affaiblis. Notre système immunitaire reconnaît quand même l’agent pathogène et produit les anticorps adaptés pour le vaincre. Le vaccin permet ainsi non seulement de développer une immunité, mais il permet de le faire avec le niveau minimum d’exposition à l’agent pathogène concerné, dans un cadre contrôlé. Les vaccins permettent aussi d’induire une immunité lorsque les infections sont les plus dangereuses, c’est-à-dire dans les premières années de la vie. C’est pour cette raison que l’on fait aux bébés autant de vaccins.
Alors est-ce moins naturel ? Tout dépend de ce que l’on entend par ce mot. Il est peu « naturel » aussi de prendre les transports en commun ou de fréquenter des centres commerciaux remplis d’inconnus transportant toutes sortes de germes, ou encore de mettre en place des vols internationaux permettant de les transporter d’un pays à l’autre. Sans vaccins, on aurait beaucoup plus d’épidémies, ce serait plus « naturel », mais pas forcément mieux. L’appel à la nature est un argument fallacieux bien connu, notamment parce que le mot « naturel » peut dire tout et son contraire. On pourrait par exemple tout aussi bien argumenter qu’il n’est pas naturel d’exposer ses enfants à des risques accrus d’infection et de mort si l’on peut les faire vacciner. Est-ce risqué de vacciner son bébé ? Oui, sans doute. Mais tout comporte un risque. Le nourrir est risqué aussi. Il peut s’étouffer, être allergique ou être victime d’une intoxication alimentaire, mais on sait que les bénéfices compensent largement ces risques. Et c’est l’exercice que je vais faire dans le tableau ci-dessous, quels sont les risques liés aux vaccins et quels en sont les bénéfices ?
Dans le cas de vaccinations pendant la grossesse, le site du CRAT fournit toutes les informations nécessaires concernant les risques des médicaments, vaccins, radiations et dépendances pendant la grossesse et l’allaitement. N’hésitez pas à le consulter en cas d’incertitude.
Tableau: Effets démontrés liés aux maladies et aux vaccins correspondants
Références
1 Roush, Sandra W., Murphy, Trudy V. and Group, and the Vaccine-Preventable Disease Table Working (2007) ‘Historical Comparisons of Morbidity and Mortality for Vaccine-Preventable Diseases in the United States’. JAMA, 298(18), pp. 2155–2163. [online] Available from: https://jamanetwork.com/journals/jama/fullarticle/209448 (Accessed 7 September 2018)
2 Atkinson, W., Wolfe, C. and Hamborsky, J. (eds.) (2015) Epidemiology and prevention of vaccine-preventable diseases 13th ed., Public Health Foundation Publications.
3 Jefferson, Tom, Rudin, Melanie and Di Pietrantonj, Carlo (2004) ‘Adverse events after immunisation with aluminium-containing DTP vaccines: systematic review of the evidence’. The Lancet Infectious Diseases, 4(2), pp. 84–90. [online] Available from: http://www.sciencedirect.com/science/article/pii/S1473309904009272 (Accessed 12 September 2018)
4 Daley, Matthew F., Yih, W. Katherine, Glanz, Jason M., Hambidge, Simon J., et al. (2014) ‘Safety of diphtheria, tetanus, acellular pertussis and inactivated poliovirus (DTaP–IPV) vaccine’. Vaccine, 32(25), pp. 3019–3024. [online] Available from: http://www.sciencedirect.com/science/article/pii/S0264410X14004320 (Accessed 28 April 2020)
5 Sun, Yuelian, Christensen, Jakob, Hviid, Anders, Li, Jiong, et al. (2012) ‘Risk of Febrile Seizures and Epilepsy After Vaccination With Diphtheria, Tetanus, Acellular Pertussis, Inactivated Poliovirus, and Haemophilus Influenzae Type b’. JAMA, 307(8), pp. 823–831. [online] Available from: https://jamanetwork.com/journals/jama/fullarticle/1355993 (Accessed 28 April 2020)
6 Tiwari, M. D., Clark, T.A., Messonnier, M.D. and Thomas, C.G. (2011) ‘Tetanus Surveillance --- United States, 2001--2008’. Morbidity and Mortality Weekly Report (MMWR), 60(12), pp. 365–369. [online] Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6012a1.htm (Accessed 10 September 2018)
7 Collins, S., Amirthalingam, G., Beeching, N. J., Chand, M. A., et al. (2016) ‘Current epidemiology of tetanus in England, 2001–2014’. Epidemiology and Infection, 144(16), pp. 3343–3353. [online] Available from: https://www.cambridge.org/core/article/current-epidemiology-of-tetanus-in-england-20012014/5F1F4B170CBE0C8BD8FEDCD99DC87659
8 Kyu, Hmwe H., Mumford, John Everett, Stanaway, Jeffrey D., Barber, Ryan M., et al. (2017) ‘Mortality from tetanus between 1990 and 2015: findings from the global burden of disease study 2015’. BMC Public Health, 17(1), p. 179. [online] Available from: https://doi.org/10.1186/s12889-017-4111-4
9 Trojan, Daria A. and Cashman, Neil R. (2005) ‘Post-poliomyelitis syndrome’. Muscle & Nerve, 31(1), pp. 6–19. [online] Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/mus.20259 (Accessed 10 September 2018)
10 Jubelt, B. (2004) ‘Post-polio syndrome’. Current Treatment Options in Neurology, 6(2), pp. 87–93.
11 Winter, Kathleen, Zipprich, Jennifer, Harriman, Kathleen, Murray, Erin L., et al. (2015) ‘Risk Factors Associated With Infant Deaths From Pertussis: A Case-Control Study’. Clinical Infectious Diseases, 61(7), pp. 1099–1106. [online] Available from: https://academic.oup.com/cid/article/61/7/1099/289804 (Accessed 11 September 2018)
12 Winter, Kathleen, Harriman, Kathleen, Zipprich, Jennifer, Schechter, Robert, et al. (2012) ‘California Pertussis Epidemic, 2010’. The Journal of Pediatrics, 161(6), pp. 1091–1096. [online] Available from: http://www.sciencedirect.com/science/article/pii/S0022347612005586 (Accessed 11 September 2018)
13 Blangiardi, F. and Ferrera, G. (2009) ‘Reducing the risk of pertussis in newborn infants’. Journal of Preventive Medicine and Hygiene, 50(4), pp. 206–216.
14 Gabutti, Giovanni and Rota, Maria Cristina (2012) ‘Pertussis: A Review of Disease Epidemiology Worldwide and in Italy’. International Journal of Environmental Research and Public Health, 9(12), pp. 4626–4638. [online] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3546780/ (Accessed 11 September 2018)
15 Kretsinger, Katrina, Broder, Karen R., Cortese, Margaret M., Joyce, M. Patricia, et al. (2006) ‘Preventing tetanus, diphtheria, and pertussis among adults: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) and recommendation of ACIP, supported by the Healthcare Infection Control Practices Advisory Committee (HICPAC), for use of Tdap among health-care personnel’. MMWR. Recommendations and reports: Morbidity and mortality weekly report. Recommendations and reports, 55(RR-17), pp. 1–37.
16 Pichichero, Michael E., Rennels, Margaret B., Edwards, Kathryn M., Blatter, Mark M., et al. (2005) ‘Combined Tetanus, Diphtheria, and 5-Component Pertussis Vaccine for Use in Adolescents and Adults’. JAMA, 293(24), pp. 3003–3011. [online] Available from: https://jamanetwork.com/journals/jama/fullarticle/201126 (Accessed 12 September 2018)
17 Rubach, Matthew P., Bender, Jeffrey M., Mottice, Susan, Hanson, Kimberly, et al. (2011) ‘Increasing incidence of invasive Haemophilus influenzae disease in adults, Utah, USA’. Emerging Infectious Diseases, 17(9), pp. 1645–1650.
18 Collins, Sarah, Litt, David, Almond, Rachael, Findlow, Jamie, et al. (2018) ‘Haemophilus influenzae type b (Hib) seroprevalence and current epidemiology in England and Wales’. Journal of Infection, 76(4), pp. 335–341. [online] Available from: http://www.sciencedirect.com/science/article/pii/S0163445317304097 (Accessed 11 September 2018)
19 Shepard, Colin W., Finelli, Lyn, Fiore, Anthony E. and Bell, Beth P. (2005) ‘Epidemiology of Hepatitis B and Hepatitis B Virus Infection in United States Children’. The Pediatric Infectious Disease Journal, 24(9), p. 755. [online] Available from: https://journals.lww.com/pidj/Abstract/2005/09000/Epidemiology_of_Hepatitis_B_and_Hepatitis_B_Virus.2.aspx (Accessed 7 September 2018)
20 Armstrong, Gregory L., Mast, Eric E., Wojczynski, Mary and Margolis, Harold S. (2001) ‘Childhood Hepatitis B Virus Infections in the United States Before Hepatitis B Immunization’. Pediatrics, 108(5), pp. 1123–1128. [online] Available from: http://pediatrics.aappublications.org/content/108/5/1123 (Accessed 7 September 2018)
21 Shepard, Colin W., Simard, Edgar P., Finelli, Lyn, Fiore, Anthony E. and Bell, Beth P. (2006) ‘Hepatitis B Virus Infection: Epidemiology and Vaccination’. Epidemiologic Reviews, 28(1), pp. 112–125. [online] Available from: https://academic.oup.com/epirev/article/28/1/112/570408 (Accessed 7 September 2018)
22 Stanaway, Jeffrey D, Flaxman, Abraham D, Naghavi, Mohsen, Fitzmaurice, Christina, et al. (2016) ‘The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013’. The Lancet, 388(10049), pp. 1081–1088. [online] Available from: http://www.sciencedirect.com/science/article/pii/S0140673616305797 (Accessed 11 September 2018)
23 World Health Organization (n.d.) ‘Hepatitis B’. World Health Organization. [online] Available from: http://www.who.int/news-room/fact-sheets/detail/hepatitis-b (Accessed 11 September 2018)
24 Wahl, Brian, O’Brien, Katherine L., Greenbaum, Adena, Majumder, Anwesha, et al. (2018) ‘Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000–15’. The Lancet Global Health, 6(7), pp. e744–e757. [online] Available from: https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(18)30247-X/abstract (Accessed 11 September 2018)
25 Henriques-Normark, Birgitta and Tuomanen, Elaine I. (2013) ‘The Pneumococcus: Epidemiology, Microbiology, and Pathogenesis’. Cold Spring Harbor Perspectives in Medicine, 3(7). [online] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3685878/ (Accessed 11 September 2018)
26 Greenhow, Tara L., Hung, Yun-Yi and Herz, Arnd (2017) ‘Bacteremia in Children 3 to 36 Months Old After Introduction of Conjugated Pneumococcal Vaccines’. Pediatrics, p. e20162098. [online] Available from: http://pediatrics.aappublications.org/content/early/2017/03/08/peds.2016-2098 (Accessed 11 September 2018)
27 Grimwood, Keith, Anderson, Peter, Anderson, Vicki, Tan, Lesley and Nolan, Terry (2000) ‘Twelve year outcomes following bacterial meningitis: further evidence for persisting effects’. Archives of Disease in Childhood, 83(2), pp. 111–116. [online] Available from: https://adc.bmj.com/content/83/2/111 (Accessed 11 September 2018)
28 Chandran, Aruna, Herbert, Hadley, Misurski, Derek and Santosham, Mathuram (2011) ‘Long-term Sequelae of Childhood Bacterial Meningitis: An Underappreciated Problem’. The Pediatric Infectious Disease Journal, 30(1), p. 3. [online] Available from: https://journals.lww.com/pidj/Abstract/2011/01000/Long_term_Sequelae_of_Childhood_Bacterial.4.aspx (Accessed 12 September 2018)
29 Diseases, Committee on Infectious (2005) ‘Prevention and Control of Meningococcal Disease: Recommendations for Use of Meningococcal Vaccines in Pediatric Patients’. Pediatrics, 116(2), pp. 496–505. [online] Available from: http://pediatrics.aappublications.org/content/116/2/496 (Accessed 12 September 2018)
30 Wolfson, Lara J., Grais, Rebecca F., Luquero, Francisco J., Birmingham, Maureen E. and Strebel, Peter M. (2009) ‘Estimates of measles case fatality ratios: a comprehensive review of community-based studies’. International Journal of Epidemiology, 38(1), pp. 192–205. [online] Available from: https://academic.oup.com/ije/article/38/1/192/696766 (Accessed 12 September 2018)
31 McLean, H. Q., Fiebelkorn, A.P., Temte, J.L. and Wallace, G.S. (2013) ‘Prevention of Measles, Rubella, Congenital Rubella Syndrome, and Mumps, 2013: Summary Recommendations of the Advisory Committee on Immunization Practices (ACIP)’. Morbidity and Mortality Weekly Report (MMWR), 62, pp. 1–34.
32 Demicheli, Vittorio, Rivetti, Alessandro, Debalini, Maria Grazia and Pietrantonj, Carlo Di (2012) ‘Vaccines for measles, mumps and rubella in children’. Cochrane Database of Systematic Reviews, (2). [online] Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004407.pub3/abstract (Accessed 7 September 2018)
33 Zamir, C. Stein, Schroeder, H., Shoob, H., Abramson, N. and Zentner, G. (2015) ‘Characteristics of a large mumps outbreak: Clinical severity, complications and association with vaccination status of mumps outbreak cases’. Human Vaccines & Immunotherapeutics, 11(6), pp. 1413–1417. [online] Available from: https://doi.org/10.1080/21645515.2015.1021522 (Accessed 12 September 2018)
34 Yung, Chee-Fu, Andrews, Nick, Bukasa, Antoaneta, Brown, Kevin E. and Ramsay, Mary (2011) ‘Mumps Complications and Effects of Mumps Vaccination, England and Wales, 2002–2006’. Emerging Infectious Diseases, 17(4), pp. 661–667. [online] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3377415/ (Accessed 12 September 2018)
35 Sugishita, Yoshiyuki, Shimatani, Naotaka, Katow, Shigetaka, Takahashi, Takuri and Hori, Narumi (2015) ‘Epidemiological Characteristics of Rubella and Congenital Rubella Syndrome in the 2012–2013 Epidemics in Tokyo, Japan’. Japanese Journal of Infectious Diseases, 68(2), pp. 159–165. [online] Available from: https://www.jstage.jst.go.jp/article/yoken/68/2/68_JJID.2014.195/_article/-char/ja/ (Accessed 12 September 2018)
36 Bayer, William L., Sherman, Frank E., Michaels, Richard H., Szeto, Isabel L. F. and Lewis, Jessica H. (1965) ‘Purpura in Congenital and Acquired Rubella’. New England Journal of Medicine, 273(25), pp. 1362–1366. [online] Available from: https://doi.org/10.1056/NEJM196512162732504 (Accessed 10 September 2018)
37 Steben, Marc and Duarte-Franco, Eliane (2007) ‘Human papillomavirus infection: Epidemiology and pathophysiology’. Gynecologic Oncology, 107(2, Supplement), pp. S2–S5. [online] Available from: http://www.sciencedirect.com/science/article/pii/S0090825807005446 (Accessed 12 September 2018)
38 Phillips, Anastasia, Patel, Cyra, Pillsbury, Alexis, Brotherton, Julia and Macartney, Kristine (2018) ‘Safety of Human Papillomavirus Vaccines: An Updated Review’. Drug Safety, 41(4), pp. 329–346. [online] Available from: https://doi.org/10.1007/s40264-017-0625-z (Accessed 14 September 2018)
39 Arnheim-Dahlström, Lisen, Pasternak, Björn, Svanström, Henrik, Sparén, Pär and Hviid, Anders (2013) ‘Autoimmune, neurological, and venous thromboembolic adverse events after immunisation of adolescent girls with quadrivalent human papillomavirus vaccine in Denmark and Sweden: cohort study’. BMJ, 347. [online] Available from: https://www.bmj.com/content/347/bmj.f5906 (Accessed 25 February 2020)
40 Grimaldi-Bensouda, Lamiae, Rossignol, Michel, Koné-Paut, Isabelle, Krivitzky, Alain, et al. (2017) ‘Risk of autoimmune diseases and human papilloma virus (HPV) vaccines: Six years of case-referent surveillance’. Journal of Autoimmunity, 79, pp. 84–90. [online] Available from: http://www.sciencedirect.com/science/article/pii/S0896841116302141 (Accessed 25 February 2020)
41 Scheller, Nikolai Madrid, Svanström, Henrik, Pasternak, Björn, Arnheim-Dahlström, Lisen, et al. (2015) ‘Quadrivalent HPV Vaccination and Risk of Multiple Sclerosis and Other Demyelinating Diseases of the Central Nervous System’. JAMA, 313(1), pp. 54–61. [online] Available from: https://jamanetwork.com/journals/jama/fullarticle/2088853 (Accessed 25 February 2020)
42 ANSM (2015) ‘Vaccination contre les infections à HPV et risque de maladies auto-immunes : une étude Cnamts/ANSM rassurante - Point d’information’. [online] Available from: https://ansm.sante.fr/S-informer/Points-d-information-Points-d-information/Vaccination-contre-les-infections-a-HPV-et-risque-de-maladies-auto-immunes-une-etude-Cnamts-ANSM-rassurante-Point-d-information (Accessed 3 April 2020)
43 INSERM (n.d.) ‘Grippe’. Inserm. [online] Available from: https://www.inserm.fr/information-en-sante/dossiers-information/grippe (Accessed 12 September 2018)
44 Santé publique France (n.d.) ‘Point sur les connaissances / Grippe?: généralités / Grippe / Maladies à prévention vaccinale / Maladies infectieuses / Dossiers thématiques / Accueil’. [online] Available from: http://invs.santepubliquefrance.fr/Dossiers-thematiques/Maladies-infectieuses/Maladies-a-prevention-vaccinale/Grippe/Grippe-generalites/Point-sur-les-connaissances (Accessed 12 September 2018)
45 Bohlke, Kari, Davis, Robert L., Marcy, S. M., Braun, M. M., et al. (2003) ‘Risk of Anaphylaxis After Vaccination of Children and Adolescents’. Pediatrics, 112(4), p. 815. [online] Available from: http://pediatrics.aappublications.org/content/112/4/815.abstract
Date de dernière mise à jour : 04/11/2021